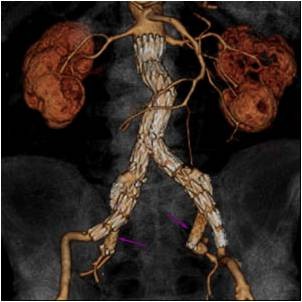
An abdominal aortic aneurysm (AAA) is a pathological increase in size of the main blood vessel in the abdomen. The normal aortic size is approximately 2 cm in men and a bit smaller in women. As the aorta increases in size, the risk of rupture increases. The condition is frequently silent and rupture can be the first symptom. Elective repair is available across Canada with significantly better outcomes when compared to those treated for aortic rupture. Abdominal aortic aneurysms (AAAs) are common and can be deadly if they are not treated. When aortic rupture occurs the majority do not survive.
Who is at Risk?
Five per cent of men and under one per cent of women over the age of 65 have an abdominal aortic aneurysm (AAA). All men between the ages of 65 and 75 and those under 65 with a family history should be screened. Women over 65 who are at high risk because of a smoking history and a family history should also be screened.
Screening
 Abdominal aortic aneurysm screening uses ultrasound technology to measure the size of your abdominal aorta. The process is painless. You lie on your back on an exam table while a technologist applies gel to your abdomen. The technologist then takes images and measurements of your aorta by moving an instrument called a transducer across your abdomen.
Abdominal aortic aneurysm screening uses ultrasound technology to measure the size of your abdominal aorta. The process is painless. You lie on your back on an exam table while a technologist applies gel to your abdomen. The technologist then takes images and measurements of your aorta by moving an instrument called a transducer across your abdomen.
This in-office screening procedure is available at Oakville Vascular. Talk with your doctor today about abdominal aortic aneurysm screening.
What is Peripheral Artery Disease (PAD)?
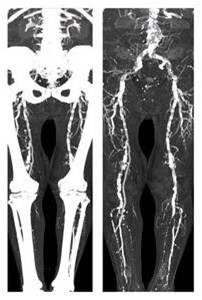
Normally the arteries carry blood away from the heart and deliver it to the body including the legs. This allows the leg muscles to exercise and work normally. PAD is a blockage in the circulation to the legs (poor circulation). This results in poor blood supply to the legs and feet which can result in leg pain or fatigue. In severe cases it can result in gangrene and amputation. PAD is a common cause of disability and is one of the more frequent manifestations of atherosclerosis or generalized vascular disease.
leg pain or fatigue. In severe cases it can result in gangrene and amputation. PAD is a common cause of disability and is one of the more frequent manifestations of atherosclerosis or generalized vascular disease.
What causes Peripheral Artery Disease?
PAD is caused by blockage in the arteries supplying blood to the legs. The cause of the blockage is atherosclerosis or "hardening" of the arteries. This is the same disease that can cause heart attacks and strokes but in this case it is affecting the arteries of the legs. Atherosclerosis occurs in the legs related to: smoking, diabetes, high blood pressure, elevated cholesterol, aging and heredity. Some of these factors can be controlled or treated, some can't.
What are the symptoms of Peripheral Artery Disease?
In it's mildest form PAD is silent, causes no symptoms and can only be detected with diagnostic testing. As PAD progresses patients develop pain or fatigue in the legs with exercise. This affects the major muscles of the calf , thigh or buttock. The discomfort usually occurs at the same distance of walking every time (consistent) and resolves within a few minutes of resting (relief). This is called claudication. When PAD is more severe there is pain even at rest and at night (usually in the foot). Skin breakdown (ulcer) or dead tissues (gangrene) can occur at this point. This is called critical limb ischemia. If this occurs there is a risk of amputation.
PAD Diagnosis and Testing
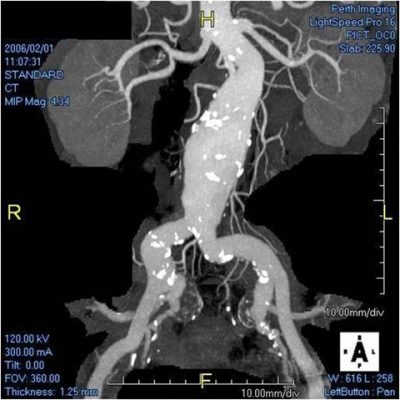
Usually a physical exam of the pulses of the leg and a simple Doppler ultrasound of the leg arteries will diagnose the presence and severity of PAD. Further testing with CT scan (a non invasive x-ray), MR scan (a non invasive magnetic scan) or an angiogram (an invasive x-ray) may be needed to plan the best treatment of PAD.
Lifestyle Modification for Peripheral Artery Disease
The most important thing for patients with PAD to do is to continue to exercise as much as they are able. Walking to the point of discomfort trains the leg muscles to work better and promotes improved circulation. It is also important to:
- stop smoking immediately
- loose weight if overweight
- diet to decrease cholesterol
- limit salt intake to decrease high blood pressure
Treatment for Peripheral Artery Disease
Our team of vascular specialists will provide you with the best treatment options based on your diagnosis.
What is Carotid Artery Disease?
The carotid arteries are the two large vessels that run up either side of the neck. They then divide into two large branches. One is the external carotid artery that supplies blood to the face and neck. The other is the internal carotid artery and it supplies blood to the eye and brain. The point at which the artery divides is slightly wider and is called the carotid bulb. Atherosclerosis, or plaque formation, seems to occur preferentially at this site, causing narrowing of the blood vessel and reduces blood flow to the brain and eye. This can result in stroke or blindness.
What causes Carotid Artery Disease?
A build up of plaque made up of cholesterol, calcium, fibrotic tissue and cellular debris called atherosclerosis thickens and narrows the arteries in the neck. Sometimes this plaque softens and breaks open. When this happens, clot-forming cells called platelets stick to the plaque. Sometimes the whole artery will clot and reduce the flow of blood to your brain causing a stroke. More often, debris from the plaque or bits of platelet plug will travel up the artery, blocking the blood vessels within the eye or brain, causing blindness or stroke.
What are the symptoms of Carotid Artery Disease?
Carotid artery disease occurs more frequently as we age and affects up to 3% of the general population. Most of the time there are no symptoms. The first symptom may be a stroke with tingling or weakness of one side of the body or face, slurred speech or difficulty speaking or sudden blindness in one eye. Sometimes these symptoms only last a short time and resolve totally. This is a mini-stroke or TIA (transient ischemic attack). Just because the symptoms go away, it is still important to seek medical attention immediately. These mini-strokes can be an early warning of impending major, permanent stroke if they are not investigated and treated.
When should I see my doctor?
If you experience sudden weakness or tingling of one of your arms, legs, or one side of your face, slurred speech or difficulty speaking or blindness in one eye, you should seek medical attention immediately, even if the symptoms completely resolve after a short time. If you smoke, have high blood pressure, diabetes, high cholesterol and/or a family history of atherosclerosis, you should see your doctor regularly for counselling and treatment of these conditions to reduce your likelihood of developing carotid artery disease.
Diagnosis and tests for Carotid Artery Disease
Your doctor will start by taking a health history and examining you. This will help determine your risk factors for developing carotid artery disease. These include smoking, high blood pressure, high cholesterol and family history. The first test your doctor will usually order is an ultrasound of the carotid vessels. This is a non-invasive test that uses sound waves to look at the carotid arteries and to assess the blood flow through them. Sometimes more information is required and a CT angiogram or Magnetic Resonance Angiogram (MRA) may be ordered. These tests involve giving contrast (dye) and use of either x-rays for CT, or magnetic fields for MRA to create a picture of the artery.
Lifestyle modification for Carotid Artery Disease
If you smoke you are very likely to develop progressive atherosclerosis. Quitting smoking will not necessarily reverse the formation of plaque in the carotid arteries but it may stop the progression of narrowing and reduce the possibility of plaque breakdown that can trigger a stroke. Other factors such as exercise, weight loss and a diet low in saturated fat can reduce the risk of developing atherosclerotic disease.
Non-surgical and Medical Management for Carotid Artery Disease
Medications that prevent platelets from sticking to the plaque surface are important in preventing stroke. The most commonly used medication for this is aspirin. A dose of 81 - 325 mg daily is recommended. If you are intolerant of aspirin, your doctor will discuss alternate medications that can be used. Studies have also shown that being on a statin agent for cholesterol control can induce remodelling and even regression of the carotid plaque. High blood pressure itself is a risk factor for stroke and developing atherosclerosis and should be treated with medication. If you are diabetic, good control of your blood sugar levels is also important.
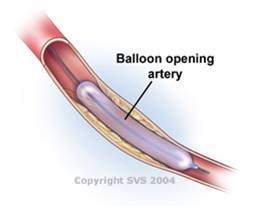
Guidelines for Intervention for Carotid Artery Disease
The goal of intervention on a carotid narrowing is to reduce your risk of stroke. If you have had a non-disabling stroke or TIA due to carotid stenosis and have over 70% narrowing, your doctor will usually recommend intervention to get rid of the narrowed area, either with surgery or angioplasty, described below. If you have symptoms and 50-69% narrowing, intervention may be recommended, but risk factor treatment and medication changes might be tried first. If you have no symptoms of stroke or TIA, the recommendation for intervention is often based on factors such as your age, degree of narrowing and medical fitness for the procedure.
Treatment for Carotid Artery Disease
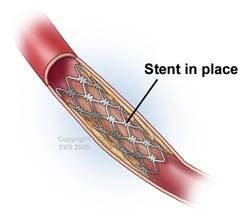
There are several treatment options available for carotid artery disease ranging from endovascular treatments including angioplasty and stenting, to surgical procedures. Our team at Oakville Vascular will provide you with the treatment options based on your diagnosis.